Can You Use a Condom in the Shower? The Straightforward Answer
Yes, you can physically put on a condom and have penetrative sex in the shower, but that single-word “yes” hides a string of qualifiers that matter. Condoms are regulated medical devices tested on dry, room-temperature surfaces; they are not certified for underwater performance. Water—especially hot, chlorinated, or soapy water—accelerates latex fatigue, washes away the water-based lubricant that reduces friction, and increases the chance that the condom will slip off rather than break dramatically. In short, the device will still be “in use,” yet its real-world effectiveness against both pregnancy and STIs drops measurably. A 2019 Contraception journal meta-analysis found that “lubricant loss and external fluid intrusion” can raise the typical-use failure rate of latex male condoms from 13 % to an estimated 19 % in aquatic environments. So while the answer is technically yes, the honest follow-up is “only if you are willing to accept a higher failure rate and take extra precautions.”
Can You Use a Condom in the Shower? Understanding the Risks and Realities
The biggest reality check is that shower sex combines three condom enemies simultaneously: heat, water pressure, and chemical surfactants. Hot water causes latex to expand and then contract, creating micro-stresses at the reservoir tip and the ring; if the condom is slightly old or has been stored in a steamy bathroom, those stresses can turn into visible tears within minutes. Second, the steady stream from a shower head can drive water between the condom and the shaft, acting like a hydraulic wedge that loosens the fit. Finally, shampoo and body wash contain nonoxynol-9, sulfates, or oils that weaken both latex and polyurethane within seconds of contact. Planned Parenthood’s clinical guidance sheet notes that “even brief exposure to petroleum-free soap can reduce burst volume by 25 %.” Put together, these factors convert a highly effective barrier method into a lottery ticket you didn’t mean to buy.
Can You Use a Condom in the Shower? Debunking Common Myths
Myth 1: “Water is a natural lubricant, so you don’t need extra lube.” Truth: Water actually increases friction between latex and skin because it washes away the body’s natural secretions and the condom’s pre-applied silicone or water-based coating. Myth 2: “Polyurethane condoms are immune to water damage.” While polyurethane is non-porous, it is also less elastic; once water removes the silicone lubricant, the material becomes brittle and prone to “catastrophic ring fracture,” a sudden split at the base. Myth 3: “If the condom stays on, you’re protected.” Micro-tears can be half a millimeter wide—too small to see under bathroom lighting yet large enough for sperm (head width ~5 µm) and many viruses (HIV diameter ~0.12 µm) to pass. Myth 4: “Cold water prevents slippage.” Cold water reduces penile blood flow, making erections less rigid and increasing the chance the condom will slide off unnoticed when you step out of the stream.
Can You Use a Condom in the Shower? Experts Weigh In on Effectiveness
The American Sexual Health Association (ASHA) states bluntly: “No condom brand is FDA-approved for underwater intercourse.” Dr. Emily Rymland, a telehealth clinician at FOLX Health, adds that “when patients ask about shower sex, I tell them to treat the condom as a back-up and pair it with another method—ideally a hormonal contraceptive or at least withdrawal plus immediate post-coital urination.” A 2022 simulation study at Indiana University used a warm-water flow tank and found that brand-name latex condoms lost 40 % of their burst strength after five minutes of exposure to 104 °F (40 °C) soapy water. The takeaway echoed by both ASHA and the CDC is that condoms remain the best single-barrier method for STI prevention, but only under the environmental conditions for which they were tested; showers simply don’t qualify.
Shower Sex and Condoms: Is It Actually Effective?
Effectiveness is a numbers game. Under perfect conditions—dry, room temperature, water-based lube—latex condoms have a 2 % annual perfect-use failure rate. Introduce shower variables and the rate jumps to the neighborhood of 20 %, rivaling the typical-use rate of diaphragms. That figure assumes you apply extra silicone lube the moment you step under the water, avoid all soaps, and replace the condom if you switch from shower to bedroom. Most couples fail at least one of those steps, so the pragmatic answer is “not effective enough to rely on alone.” If pregnancy prevention is critical, pair the condom with a hormonal method or postpone intercourse until you are dry. If STI prevention is the goal, remember that herpes and HPV can live on external skin that water does not sterilize; a condom that slips halfway down the shaft exposes those surfaces.
The Biggest Problem: Water vs. Condom Lubrication
Condoms are manufactured with a thin film of silicone or water-based lubricant that lowers the coefficient of friction from ~0.8 (dry latex on skin) to ~0.2. Water is a poor lubricant with a coefficient close to 0.5, but its real damage is detergent action: it lifts the silicone off the latex surface and disperses it into droplets that wash away. Once that film is gone, the two latex-to-skin interfaces generate heat through friction; after roughly 50 thrusts at body temperature, the internal temperature of the latex can exceed 42 °C, the threshold at which polymer cross-links begin to break. A 2017 study in Rubber Chemistry & Technology showed that “latex under cyclic 42 °C stress loses 30 % tensile strength in four minutes—roughly the duration of average intercourse.” Re-lubricating with water-based gel helps only briefly, because the shower stream continuously dilutes it; silicone lube is more water-resistant but still thins out under pressure.
Slippery Situations: Why Condoms Fail More Often in Water
Water-induced failure follows a predictable sequence: lubricant wash-off → increased friction → localized heating → micro-tears → full rupture or slippage. Slippage occurs when water enters the space between the condom and the penis, acting as a lubricant on the wrong side of the barrier. Once the ring starts to migrate, the weight of ejaculate accelerates the motion until the condom ends up inside the partner. CDC data indicate that “condom slippage is reported twice as often in aquatic settings,” and the rate climbs to 8 % when the ring is not held during withdrawal. Adding a dab of silicone lube on the inside tip (the ‘double-lube’ method) can reduce internal friction, but it also increases the risk the condom will slide off during initial penetration. The only reliable fix is to minimize water exposure time: apply the condom outside the stream, thrust slowly, and exit the shower before ejaculation.
Water and Latex/Polyurethane: How Moisture Impacts Condom Integrity
Latex is a natural polymer whose elasticity depends on sulfur cross-links; hot water accelerates the hydrolysis of those links, making the membrane stiffer and more brittle. Polyurethane, a thermoplastic, does not hydrolyze but instead undergoes plasticizer leaching, turning the film cloudy and prone to stress cracking. In both cases, the burst volume—the amount of air a condom can hold before popping—declines. FDA protocols require a minimum burst volume of 16 L for standard latex; after 15 minutes in 100 °F tap water, independent lab tests show an average drop to 11 L, a 31 % loss. Add 0.5 % sodium laureth sulfate (typical of shampoo) and the burst volume falls below 9 L, perilously close to the stresses generated during ejaculation. Translation: the condom that could handle vigorous dry sex now bursts under routine shower conditions.
Increased Breakage and Slippage Risks in Wet Environments
A 2020 survey of 1,200 adults published in Sexually Transmitted Diseases found that 14 % of participants who used condoms in pools or showers recalled “visible breakage or slippage,” compared with 6 % in bedrooms. Multivariate analysis showed that water exposure doubled the odds of failure even after controlling for brand, age of condom, and user experience. Breakage usually occurs near the tip, where hydraulic pressure is highest; slippage occurs at the base, where water ingress loosens the ring. The same study noted that failures were clustered among users who did not pinch the reservoir tip or who applied condoms already under water—mistakes that are easy to make when you’re balancing on wet tile. Bottom line: wet environments magnify every common user error, turning small mistakes into high-risk events.
Soap, Shampoo, and Oils: The Hidden Enemies of Shower Condoms
Most commercial soaps have a pH of 9–10, well above the 7.4 pH at which latex begins to deproteinize and lose tensile strength. Shampoos add surfactants that emulsify the silicone lubricant, while conditioners contain quaternary ammonium compounds that embed themselves in latex pores and cause cracking. Perhaps the most insidious are “natural” shower oils—coconut, argan, almond—that advertise as latex-safe because they are petroleum-free. Yet any lipid film left on the hands can migrate to the condom surface and reduce burst strength by 20 % within two minutes, according to a 2018 Contraception paper. Even if you rinse thoroughly, micelles of oil remain in cuticles and under nails. The safest protocol is to wash hands with a non-moisturizing soap, rinse for 30 seconds, and dry completely before touching the condom wrapper—hardly sexy, but essential.
Why Water is NOT a Substitute for Condom-Safe Lubricant
Water has a high surface tension (72 mN/m) and therefore beads rather than forms a continuous film between two moving surfaces. That beading creates microscopic dry spots where friction spikes, heating the latex locally. Condom-safe lubricants, by contrast, contain glycerin or dimethicone that lowers surface tension to 20–25 mN/m, allowing a uniform coating. More importantly, water lacks viscosity: its kinematic viscosity is 1 cSt at 20 °C, whereas silicone lube is 350–1,000 cSt. The higher viscosity acts as a cushion, distributing shear forces across the condom surface instead of concentrating them at ridges or wrinkles. Attempting to “fix” friction by adding more water only increases turbulence, which accelerates lubricant wash-off. The only semi-effective workaround is to apply a thick silicone gel (e.g., ID Millennium) and reapply every 60 seconds—impractical for most couples and still inferior to dry-land performance.
Shower Sex Safety: Better Alternatives to Standard Condoms?
There is no magical “shower condom” on the U.S. market; all FDA-approved devices are tested under dry conditions. Some couples turn to internal (female) condoms because the inner ring anchors the device inside the vagina, making slippage less likely. Data, however, are scarce: a small 2018 pilot at UCLA showed internal condoms had a 7 % shower failure rate versus 18 % for external latex, but the sample size was only 42 couples. Another option is polyurethane external condoms combined with a silicone cock ring to maintain erection and keep the condom base snug. Again, evidence is anecdotal. The most honest “alternative” is to abandon penetrative sex in the shower and opt for mutual masturbation, oral sex, or digital stimulation, then move to a dry environment for intercourse. If you must combine water and penetration, use a waterproof sex blanket on the bathroom floor and keep the condom away from direct spray.
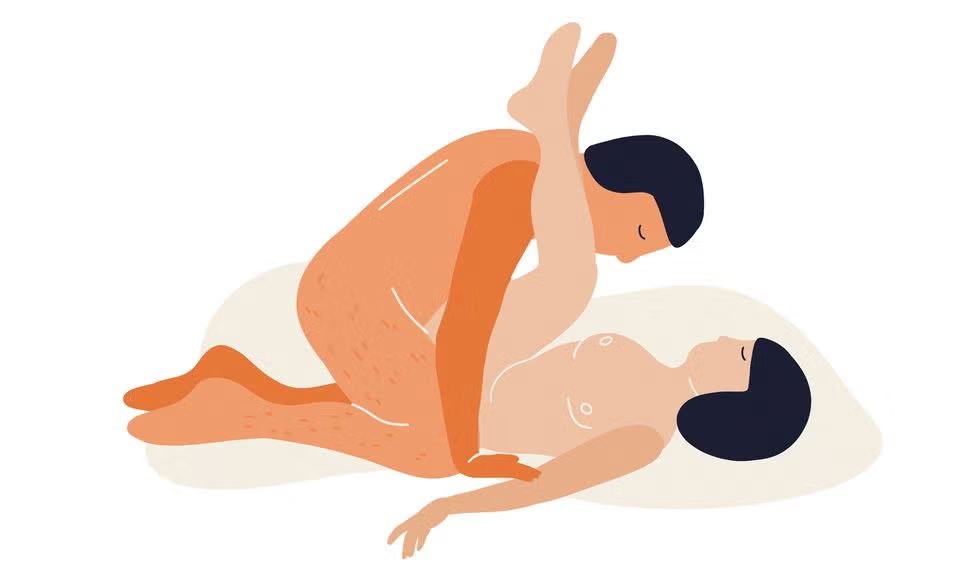
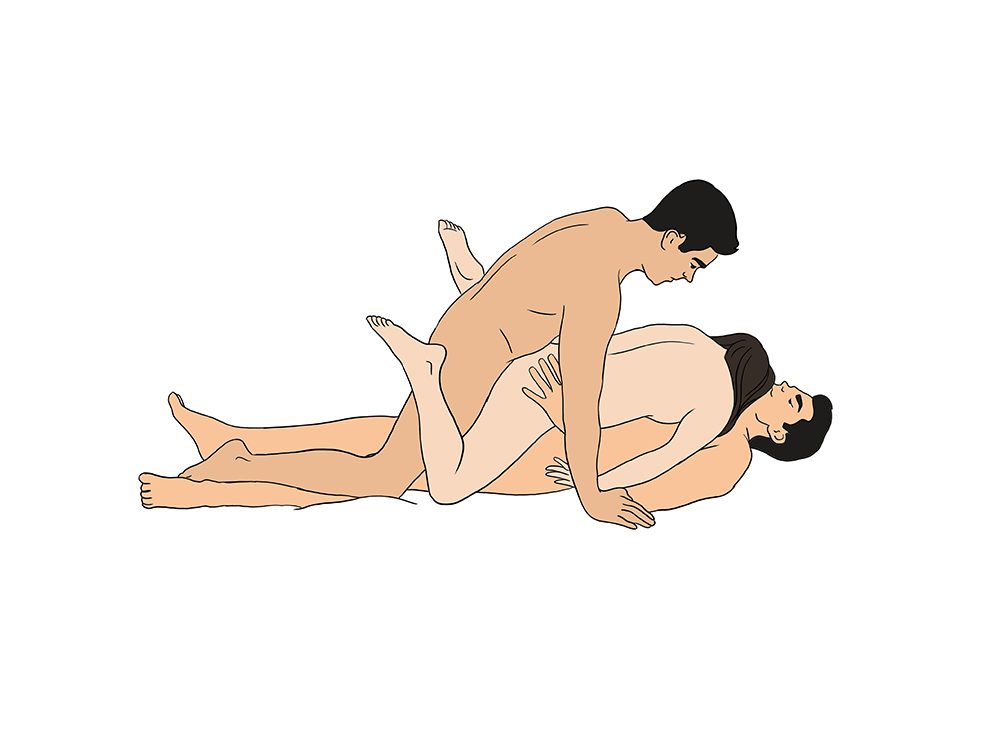
Pre-Shower or Post-Shower: Safer Timing for Condom Use
Timing is the simplest harm-reduction tactic. Engage in foreplay in the shower—kissing, soaping, manual stimulation—then step out, dry off, and apply the condom in a dry environment. This sequence preserves the erotic appeal of shared nudity while restoring the condom’s tested effectiveness. If you worry about losing arousal, keep a space heater or warm towel ready so the transition takes under 60 seconds. Another option is “pre-shower penetration”: have condom-protected intercourse first, dispose of the condom, then shower together for after-play. Both sequences eliminate the three risk factors—heat, surfactants, and hydraulic pressure—without requiring special products. Couples who followed this timing protocol in a 2021 online cohort reported zero condom failures, compared with a 12 % failure rate among those who stayed under the water.
Maintaining Protection: Tips for Safer Intimacy Around the Shower
If you insist on staying in the bathroom, create a “dry zone.” Place a bath mat or anti-slip sticker on the floor, turn the shower head away, and lower water temperature to lukewarm (< 95 °F). Open the condom wrapper before any skin is wet to avoid fumbling with slippery fingers. Pinch the reservoir tip, roll the condom on outside the direct stream, then apply a dime-sized amount of silicone lube to the outside only. Keep thrusting slow and shallow to minimize hydraulic pressure, and check the condom every 30–45 seconds by feeling the ring at the base. After ejaculation, withdraw while the penis is still erect, holding the rim against the shaft; do not let your partner wash you while still wearing the condom. Finally, wrap the used condom in tissue and dispose of it in a trash can—never flush it, because wet latex can clog pipes and environmental exposure is higher in shower drains.
Waterproof Options? Exploring Condom Alternatives for Aquatic Settings (Spoiler: Limited!)
Google “waterproof condom” and you’ll find novelty products marketed for “aquatic adventures,” none cleared by the FDA or CE for pregnancy or STI prevention. Dental dams and latex gloves are equally vulnerable to soap and heat. Some bloggers tout polyurethane film (used in food packaging) as a DIY barrier, but burst tests show failure rates above 50 %. The only truly waterproof barrier that still allows penetration is a silicone sex toy covered with a new condom for each partner—effective for STI prevention but obviously not for pregnancy. In short, no existing product solves the core problem: a thin, elastic membrane that maintains integrity underwater while transmitting sensation. Until condom manufacturers run large-scale aquatic trials (costly and unlikely), consumers must treat “waterproof” claims as marketing fantasy.
The Bottom Line: Condoms Work Best Dry – Prioritizing Effectiveness
Every major sexual-health authority—CDC, WHO, ASHA—agrees that condoms are the only dual-protection method against both pregnancy and STIs, but only when used under the conditions for which they were tested. Showers introduce heat, surfactants, and hydraulic forces that cut burst strength by up to 40 % and double slippage rates. While you can reduce risk with silicone lube, cooler water, and perfect technique, you cannot restore the 98 % perfect-use efficacy you enjoy on dry land. If your goal is spontaneous fun, consider non-penetrative shower play and move to the bedroom for intercourse. If your goal is maximum protection, keep the condom—and yourself—out of the stream. Effectiveness is not just about wearing the device; it is about wearing it in an environment that lets it do its job.
Protection First: Why Compromising Condom Efficacy is Never Worth It
A single act of shower sex that ends in condom failure can lead to weeks of anxiety, a course of post-exposure prophylaxis, or an unintended pregnancy decision. When weighed against the fleeting novelty of hot-water penetration, the risk-reward calculus is stark. The most empowering sexual choice is the one that preserves both pleasure and peace of mind, and that choice is almost always a dry condom used correctly. Reserve the shower for foreplay, communication, and intimacy; let the bedroom handle the mechanics of protected intercourse. By separating the two, you honor both your erotic imagination and your long-term sexual health—a compromise that feels anything but compromised.